Can care coordination software really help hospitals improve revenue?
With the COVID-19 pandemic causing unprecedented disruptions to the healthcare industry, hospitals and health systems have been struggling to stay afloat amidst declining revenues and rising costs. Care coordination software may help address some of the financial challenges these organizations face.
Hospitals have struggled financially in recent years, and 2022 was the worst operating year ever for them. One of the biggest challenges hospitals face is the rising cost of wages exceeding the point of profitability. High turnover rates and staffing shortages have further increased the cost and demand for qualified healthcare workers.
In addition, many hospitals are experiencing poor Medicaid payments, which often fail to cover the total cost of treatment. These financial challenges have put pressure on hospitals to find new ways to improve revenue and cut costs.
In this article, we will explore some of the key ways in which care coordination software can help hospitals improve revenue and achieve their financial goals. From reducing readmissions to improving patient outcomes and enhancing operational efficiency, we’ll explain how healthcare organizations can leverage care coordination software to deliver high-quality, patient-centered care.
Care Coordination Software Enhances the Patient Experience
1: Improve Patient Outcomes
Ensuring excellent patient outcomes is a top priority for hospitals, because this is the key indicator to reflect high-quality care. By always aiming to improve patient outcomes, hospitals can improve their reputation and, in turn, increase revenue.
Empowering patients to take an active role in their health is a crucial step toward improving health outcomes. When patients are engaged in their healthcare journey, they’re more likely to make informed decisions and follow through with care plans. This can also help minimize appointment no-shows, increase patient satisfaction, and reduce healthcare costs.
Care coordination software plays a vital role in enhancing patient engagement. By simplifying the sharing of PHI and facilitating provider communication, care coordination software fosters a collaborative and patient-centered care approach.
2: Ease Population Health Management
Population health management involves identifying and addressing the health needs of a community to improve outcomes and reduce healthcare costs. This is a daunting task that requires the collaboration of medical professionals across large networks.
Care coordination software helps hospitals streamline population health management by enabling providers to discuss patient treatment across multiple care settings. This allows providers to develop proactive care plans and interventions to address serious issues before they get worse.
Another benefit of Care coordination software in population health management is the ability to monitor patient health data in real-time. By collecting and analyzing new medical records, providers can track patient progress, identify trends, and make informed decisions about care. This can help prevent complications and ensure that patients receive the appropriate care at the appropriate time.
3: Boost Patient Satisfaction
Patient satisfaction is a critical component of the success of any healthcare organization. Happy patients are more likely to return for future care and recommend the organization to others. In contrast, unsatisfied patients are more likely to seek care elsewhere and leave negative reviews. This can hurt an organization’s reputation and financial success.
However, improving patient satisfaction is not always easy. Patients have high expectations for their healthcare experience, and there are numerous factors that can impact their satisfaction, including wait times, poor communication, and lack of control over their care. Additionally, the increasing demand for healthcare services and the growing complexity of patient care can make it challenging for hospitals to provide efficient, personalized care.
Care coordination software helps care teams communicate more effectively and meet the unique needs of each patient. Patients want to have power and transparency in their care, and this solution can help your organization provide it.
4: Enhance Care Transitions
Care transitions, or the movement of patients from one healthcare setting to another, can be a vulnerable time for patients. However, care coordination software can help improve care transitions by providing a centralized platform for managing patient information.
With Care Coordination Software, healthcare providers can track patient progress throughout the care continuum, including hospital stays, rehabilitation, and home care. This can help providers identify gaps in care and intervene earlier to prevent complications or readmissions. Additionally, Care Coordination Software can facilitate communication between providers, ensuring that patients receive the right care at the right time.
Care Coordination Software Reduces Redundancy
5: Reduce Readmissions
Readmission to the hospital within 30 days of discharge is a significant concern for patients and healthcare providers. Not only can it be stressful for patients and their families, but it can also be costly for hospitals.
Readmissions can occur due to a variety of reasons, such as incomplete discharge instructions, lack of follow-up care, or medication errors. When patients are readmitted to the hospital, it can lead to increased healthcare costs, lower patient satisfaction, and increased risk of complications.
Care coordination software can help hospitals reduce readmissions with collaborative care and patient support. Care coordination software can also help providers monitor patients’ progress and intervene early if there are any warning signs.
6: Minimize Duplication of Services
Duplication of services is a common issue in healthcare that raises costs without necessarily improving the quality of care. A lack of coordination among care teams is the main reason for patients to undergo unnecessary tests and treatments. Using care coordination software helps keep each provider involved in a patient’s health on the same page.
Care Coordination Software can help hospitals to minimize duplication of services by providing a centralized platform for sharing patient data and care plans. By minimizing duplication of services, hospitals can save time and resources and deliver better care to patients.
By leveraging care coordination software to minimize duplication of services, hospitals can deliver informed care and achieve financial success. This offers several benefits, including:
- Save time and resources by minimizing unnecessary tests or procedures.
- Improve patient safety by eliminating risks and adverse events from unnecessary tests or procedures.
- Enhance your reputation by providing an excellent patient experience and receiving positive reviews.
7: Prevent Medical Errors
Preventing medical errors is a critical component of delivering high-quality care. Medical errors can have serious consequences for patients, including prolonged hospital stays, additional treatments, and in some cases, even death. Medical malpractice incidents can be devastating for everyone involved, so it’s crucial to prevent avoidable errors.
One way that care coordination software can help prevent medical errors is by providing a comprehensive view of a patient’s health information. This allows providers to quickly identify potential risks and make informed care decisions.
Additionally, the ease of communication offered by care coordination software can alert providers to potential drug interactions, allergies, and other issues. By facilitating communication between providers, care coordination software enables providers to work together to develop comprehensive treatment plans.
Care Coordination Software Streamlines Operations
8: Enhance Operational Efficiency
Care Coordination Software can automate many manual processes, such as scheduling appointments and sending reminders to patients. By automating these tasks, care teams can focus on high-value activities, such as providing exceptional care.
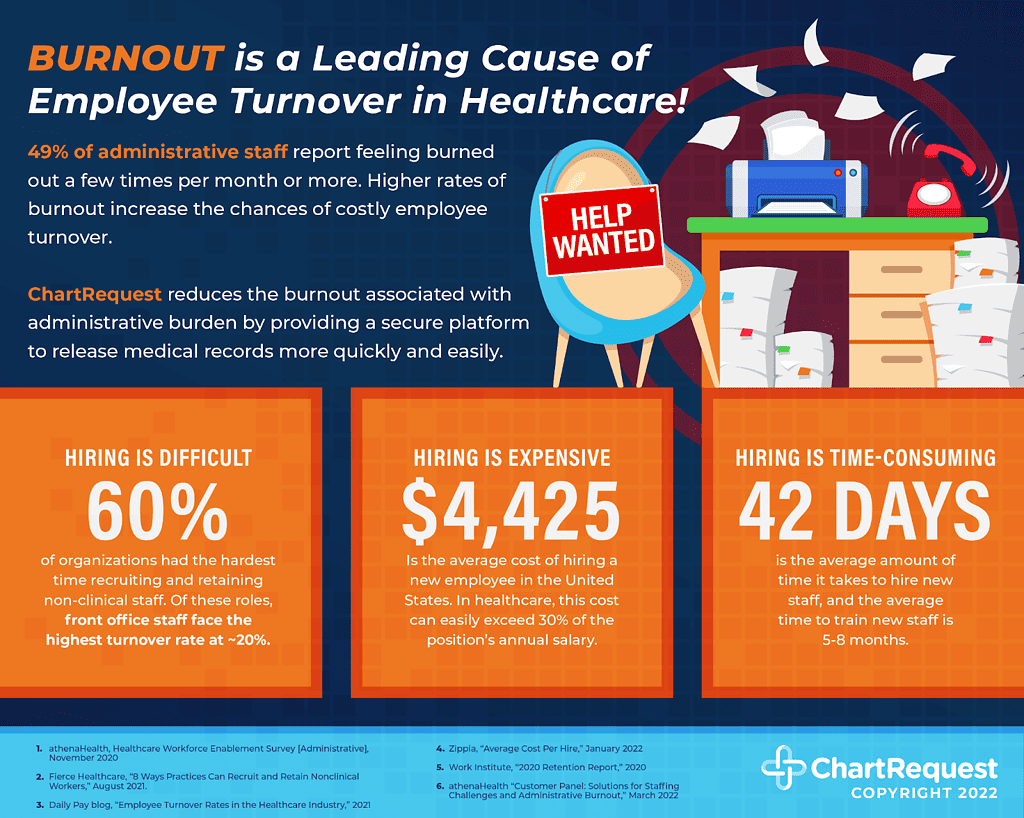
According to the 2022 NSI National Healthcare Retention & RN Staffing Report, the average hospital worker turnover rate in 2021 was 25.9%. Providing solutions to administrative burdens like care coordination software can ease the burdens driving qualified staff away.
9: Enable Value-Based Care
Value-based care is a healthcare model that aims to improve patient outcomes while reducing costs. Unlike traditional fee-for-service models, value-based care rewards providers based on the quality of care they provide, rather than the quantity of services rendered. However, implementing a value-based care model can be challenging, especially for healthcare facilities that rely on outdated, manual processes.
Care coordination software can help healthcare providers implement a value-based care model by providing a comprehensive platform for managing patient care. This can help providers identify gaps in care, improve care coordination, and ultimately improve patient outcomes while reducing costs.
In addition to these benefits, care coordination software can help providers comply with value-based care regulations and reporting requirements. With the streamlined ability to collect and analyze patient data, providers can demonstrate the quality of care they provide and qualify for value-based care incentives.
How Can Care Coordination Software Help Your Organization?
Care coordination software provides a powerful tool for healthcare organizations to improve care coordination, reduce costs, and enhance patient outcomes. By leveraging technology to streamline communication and information sharing among providers, care coordination software can help ensure that patients receive the right care at the right time, no matter where they are in the healthcare system.
ChartRequest is a digital release of information and care coordination platform that streamlines the process of requesting, processing, and fulfilling medical record requests. By eliminating manual processes and reducing administrative burdens, ChartRequest allows healthcare organizations to focus on delivering high-quality care and improving patient outcomes.
In today’s complex healthcare landscape, care coordination is more important than ever. With the right technology and tools, healthcare organizations can streamline care coordination, reduce costs, and deliver better outcomes for patients. Learn more about ChartRequest today.


